For this month’s entry I would like to pivot to writing about one of the specific disorders that patients have asked me to discuss. The goal here is not to give individual medical advice but to help you understand these disorders and how they might be impacting your overall health. Even if you personally are not dealing with a particular disorder, you likely have a wife, a daughter, a mother, a sister or a friend who might benefit from the information I will be sharing.
The first topic I would like to discuss is Polycystic Ovarian Syndrome (PCOS). I selected PCOS because I have found it to be a prevalent problem in my Gynecology practice as well as in the general population. While it often goes undiagnosed, it is the most common reproductive disorder in the world. PCOS is a condition whose primary signs are irregular menstrual cycles due to failure to ovulate (anovulation), male pattern hair growth (hirsutism) or balding and multiple small cysts on the ovaries. Not all women have all three signs but any two of the three make the diagnosis. The reason understanding PCOS is so important is that it is associated with a number of other medical problems including infertility, acne, obesity, type 2 diabetes, heart disease and hypertension.
Anovulation
The most common initial presentation of those with PCOS is irregular periods due to anovulation. Irregular cycles are very common in early adolescence so it is important to delay a diagnosis of PCOS until at least three years after the onset of menses unless the other two signs are present. In the normal menstrual cycle, only one follicle progresses from what is called a primordial follicle to a mature follicle which is released by the ovary (ovulation). In PCOS, multiple primordial follicles start the process but are unable to complete it due to an excess of the male hormone testosterone. These arrested follicles form tiny cysts that can be seen on USG. The failure of even a single egg to reach maturity in some or all cycles is the reason why so many women with PCOS may have difficulty becoming pregnant. Those enlarged ovaries have also been known to cause chronic pelvic pain.
The traditional treatment for the irregular cycles has been oral contraceptive pills (ocp’s) to suppress the ovaries and provide the patient with regular, although artificial periods. This works fine for the woman not desiring pregnancy but does not get to the root cause of the problem. Moreover, ocp’s and other hormones may not be acceptable to all women for a variety of reasons.
In the woman desiring pregnancy, the traditional treatment of PCOS has been with powerful ovulation induction drugs which work for a significant percentage of women and help them to become pregnant. However, some of these drugs are not well tolerated and have some potentially dangerous side effects. More recently doctors have added the diabetes drug metformin to treat anovulation to increase the likelihood of ovulation and pregnancy (more on why this strategy works later).
Hirsutism
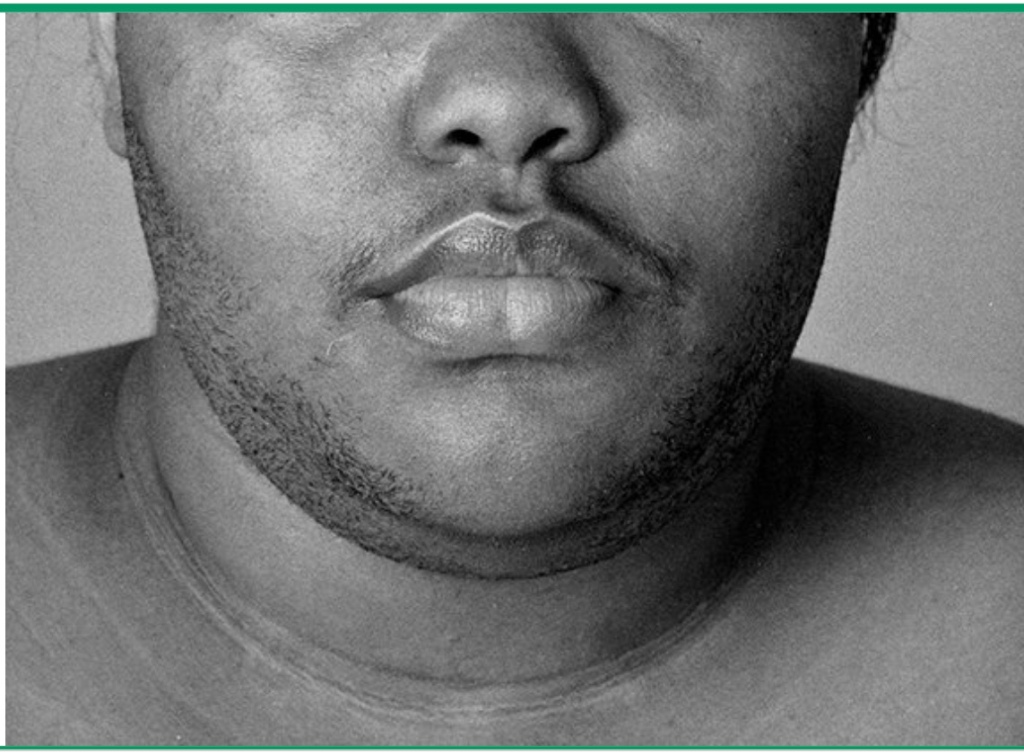
Male pattern hair growth and/or balding along with acne are visible manifestations of excess male hormones (androgens), primarily testosterone, produced by the ovaries in PCOS. Here again treatments with OCP’s and other drugs to block the effects of the androgens treat the symptoms but do not get to the root of the problem. Neither do electrolysis and other hair removal medications and procedures. These can successfully get rid of unwanted hair but do not inhibit regrowth.
Polycystic Ovaries
Now that we can easily see very small cysts in the ovary on ultrasound we can use such studies to contribute to the diagnosis of PCOS. In spite of the name, having ovaries with multiple cysts does not necessarily mean that a woman has PCOS because they can be present in normal women and not all women with multicystic ovaries have PCOS. It is only when the cysts are accompanied by excess facial hair, thinning scalp hair and/or irregular menstrual cycles that the diagnosis is made.

PCOS and Insulin Resistance
No single cause has been identified for PCOS but we do know that there is a genetic predisposition, making it more likely to occur in daughters and sisters of women with the condition. PCOS is often linked with both obesity and Type 2 diabetes although neither condition is considered to be the direct cause of PCOS. Greater than 50 to 70 percent of women with PCOS are overweight or obese and there is a markedly increased risk for the development of diabetes in women who have PCOS. In fact it is recommended that women diagnosed with PCOS be screened for diabetes at diagnosis and every two years thereafter. Recent research has confirmed that the common denominator for these three conditions; obesity, diabetes and PCOS appears to be insulin resistance.
Insulin resistance is a condition in which the pancreas can produce insulin normally but the insulin does not function properly. Insulin is the hormone responsible for moving glucose out of the blood and into the cells where it can be used for energy. When the insulin does not do that effectively, the body responds by releasing more and more insulin leading to hyperinsulinemia (elevated blood insulin levels). High insulin levels signal the body to store fat rather than burn it, leading to weight gain and obesity and making it difficult to lose weight. When insulin resistance is at work, the excess fat is stored primarily in the midsection. This increased abdominal circumference is a risk factor for multiple metabolic diseases. High insulin levels are a precursor to prediabetes and diabetes because even though a lot of insulin is being produced, it is unable to perform its main function of lowering blood sugar. In addition, high blood insulin levels can trigger the increase in male hormones produced by the ovaries that cause the anovulation, hirsuitism and acne seen in PCOS.

This link between PCOS and insulin resistance explains why metformin, a drug used to treat diabetes, can be useful in the management infertility caused by PCOS. One of the mechanisms of action of the drug is to reduce insulin resistance which results in a decrease in testosterone and a higher likelihood of normal ovulation. Some infertility specialists now use metformin alone over traditional ovulation induction drugs as the first line treatment for anovulation in patients with PCOS.
In addition to the medications previously discussed, doctors are also recommending lifestyle changes that can result in significant improvement in symptoms of PCOS. These lifestyle choices are aimed at decreasing insulin levels and improving insulin resistance. Those efforts include weight loss when appropriate, increased physical activity and dietary changes.
Weight loss, whether it is achieved by lifestyle changes in diet and exercise, medications or bariatric surgery results in decreased insulin resistance. As little as a 15% reduction in weight can improve symptoms. The same can be said for regular physical exercise which increases muscle mass which improves insulin resistance even when not associated with weight loss.
Dietary strategies to improve PCOS focus on lowering insulin levels which indirectly lowers androgen secretion by the ovaries. This involves reducing or eliminating the consumption of sugar and simple carbohydrates (bread, potatoes, pasta, rice, etc.) and processed foods. These foods are known to spike glucose and insulin levels and increase insulin resistance. Such a low carbohydrate way of eating should focus on eating foods with a low glycemic index which means they are less likely to spike glucose and insulin levels. These would include complex carbohydrates like green and cruciferous vegetables as well as protein sources like meat, fish, poultry, and eggs and healthy fat like nuts avocado and olive oil. Dietary changes that improve insulin resistance should also focus not only on what to eat but when to eat as well. Another strategy to keep insulin levels low is to avoid snacking between meals and late night eating by practicing time restricted eating or intermittent fasting (see previous blog entry).
Because PCOS is associated with so many more dangerous health conditions, any woman who believes she might have it should see her healthcare professional for a diagnosis and close monitoring. The sooner the diagnosis is made and treatment and lifestyle changes are adopted, the more likely the woman with PCOS is to reverse her risk of conditions that might impair her long term health and quality of life.
Be Blessed,
Yvonne Moore, MD
“Dear friend, I hope all is well with you and that you are as healthy in body as you are strong in spirit.” 3 John 1:2 (NLT)
Leave a comment